Bariatric surgery, weight loss and food
I recently decided to go down a surgical approach to weight loss, specifically gastric sleeve surgery, and I wanted to talk about my thought process before, "during" and shortly after

Ever since I was in school, my size and weight has been a source of embarrassment and difficulty. I was teased relentlessly for being overweight from being 5 or 6 years old onwards, and even well-meaning comments from parents of my friends about "puppy fat" are damaging enough to stick with me 30-odd years later. Emotional scars have always been significant, and deep, but over the years I've come to care less about my appearance (though I tend to walk around in a constant state of feeling uncomfortable and embarrassed) and more about my health.

It feels like I've tried a thousand different ways to try and reduce my weight and size with diet, exercise, combinations of the two; through restricting calories or carbs or sugar or a number of other ways. The long-term trend has always been upwards; short term weight loss led to no real change in the upward slope of my weight in my adult life. Having thought long and hard about my health I had decided to investigate bariatric surgical procedures.
I went in to the consultation with a gastric balloon or band in mind as possible options; having done my research on the various procedures I thought they would strike the best balance between risk, expected outcomes (which is typically measured in % excess weight loss, or EWL) and invasiveness.
| Procedure | Description | x̅ EWL (6 mo) | x̅ EWL (12 mo) | x̅ EWL (24 mo) |
|---|---|---|---|---|
| Gastric balloon | A temporary balloon inserted into the stomach to fill space and make you feel more full | 25% [1] | n/a | n/a |
| Gastric band | An adjustable band placed around the top of the stomach to create a pouch to feel full faster | 30% [2] | 40% [2] | 50% [2] |
| Gastric sleeve | ¾ of the stomach is removed, leaving a smaller banana-shaped stomach. | n/a | 49% [3] | 61% [3] |
| Gastric bypass | A small pouch is created at the top of the stomach and then connected directly to the small intestine to leave a much smaller stomach | n/a | 61% [3] | 61% [3] |
[1] https://www.sciencedirect.com/science/article/pii/S204908012100087X
[2] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3671103/
[3] https://www.sciencedirect.com/science/article/pii/S1743919116311165
My consultant talked through the procedures in some detail, and with me weighing in at the kingly figure of 160kg at 1.82m, my long-term health was clearly a huge concern. I'm lucky to still be moderately active with no heart, blood pressure or diabetes problems, but at 37 it felt a bit like the last chance to do something like this, recover and gain the long term benefits before my health deteriorated from carrying the excess weight.
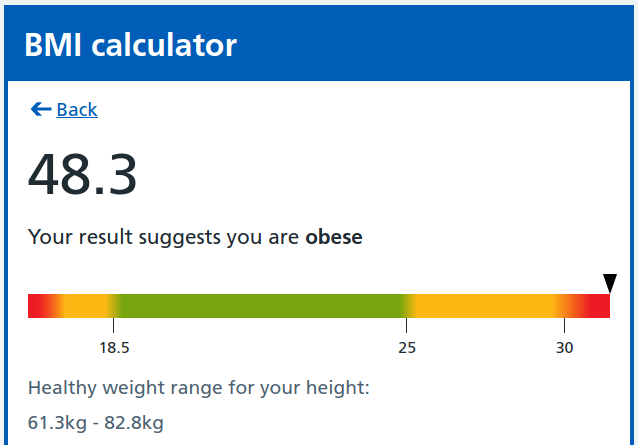
At least half of my body weight is excess weight, negatively impacting my health. Given the amount of weight needing to be lost and with no diabetes, my consultant recommended a laproscopic sleeve gastrectomy, where around ¾ of my stomach would be removed via keyhole surgery, also removing the Ghrelin-producing area of the stomach which reduces hunger as well as feeling full much faster with a significantly smaller stomach.
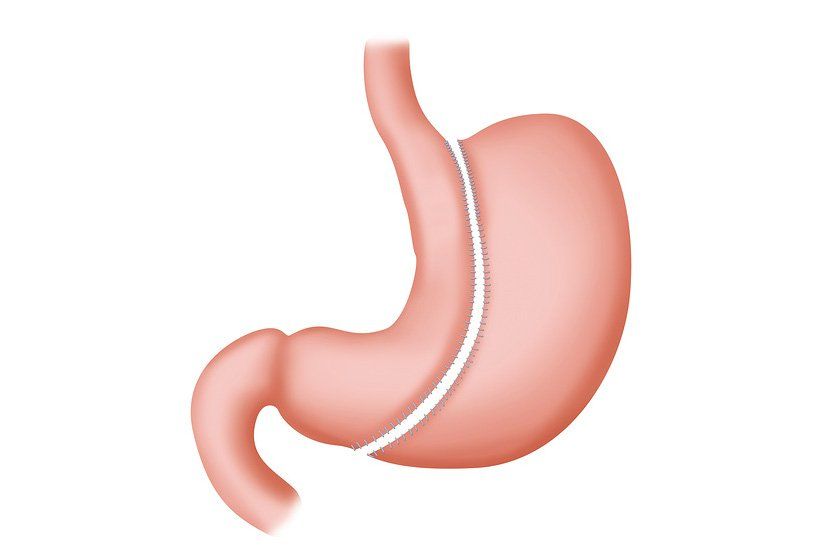
Combined with dietician support post-surgery, it is reasonably common for the mean EWL of 49% in 12 months to reach 75% or more EWL - this is a similar outcome to the gastric bypass but with around half the risk factors associated with the bypass. I took some time to consider it (given that it was a more invasive procedure, and more permanent than a gastric band technically is), talking it through with my wife in particular. Once I'd decided to go ahead, it was then the case of booking the surgery in for about 3 and a half weeks later.
Pre-op diet
The pre-op diet is a "liver-shrinking" regime, designed to reduce the fatty tissue around the liver to make it easier to lift during a keyhole procedure. I'd gone through this before when I had my gall bladder removed in 2017, but just on the basis of it being 800kcal a day - this time, I was advised to go to a more prescriptive way of getting those 800kcal based on prior success:
- Two pints of semi-skimmed milk
- 4-6 low fat yoghurts
- A salty drink (I became quite partial to a cup of Bovril, which may as well be a cup of gravy)
- A-Z multivitamin and extra calcium (these are for life now)
- Loads of water
I also cut out fizzy drinks entirely, they're very much not recommended after a gastric sleeve (because the air expansion puts pressure on the surgical staples around the stomach and that can lead to leakage into the abdomen). I did this for 3 weeks and it went pretty well - I didn't really feel hungry or weak after the first couple of days, I just wanted to eat because I missed it - this is pretty much a precursor to having to re-work my relationship with food.
The procedure
Due to COVID-19 protocols I was admitted to hospital on my own, taken to a side room to prepare and then taken down for surgery. This involved lying on a specially designed operating table and given a general anaesthetic; the procedure itself is taken with the table tilted completely upright to make access easier for the surgeon. The next thing I remember is waking up back in my room.

As my stomach capacity is so greatly reduced, post-surgery I was limited to 25ml per hour of water for the first day (as well as IV fluids and painkillers). After mostly sleeping for the first day and then being allowed to drink more fluid (within reason) I was able to stomach a small cup of milk the next morning, and recovery had begun.
Recovery
I spent a day in UHCW where I'd had the procedure before being transferred to the BMI Meriden hospital where I had arranged the procedure. After being transferred I was able to drink a mug of soup, which was the first "food" I felt I'd had in weeks at that point - but taking anything in was still somewhat of a challenge, with a strong feeling of air escaping back up whenever I swallowed and definitely being heavily restricted by stomach capacity. Luckily I was able to escape severe vomiting, which is unfortunately a reasonably common side-effect of the surgery in the first few days.
After a total of 3 nights in hospital, I was able to come home and continue to recover there, continuing on a liquid-only diet (this is essential for the first 3 weeks when the surgical staples are healing around my stomach). Pain management has been challenging; I've been in quite a lot of pain but I'm currently managing it with paracetamol and codeine, but things improve every day.
Food
In total I've been on what effectively amounts to a liquid-only diet for 4 weeks, and my general apathy to food is quite startling - I've started to dread eating entirely, and the options are so limited that I've started to resent them. I'm hoping that once the 3 weeks post-surgery are over and I can move onto pureed food that I can add a lot more variety back in and enjoy eating again; I've always enjoyed food and it would be a shame if I were to lose that, but it is also something I would accept if it helps me live a long happy life with my family and friends.